
During a presentation on moisture management at the Better Buildings: Better Business conference this past week in Wisconsin Dells, WI, a builder asked this question:
“Given the Relative Humidity Optimum Zone table everyone cites [Sterling et al, 1986; Environmental Health Perspectives Vol 65, pgs. 351 – 361; see main image], should we be running the relative humidity (RH) in our homes higher, say 50% to 70%?”
Authors’ note: The image above is a slide from a presentation from AHRI. For more on the latest in humidity research in buildings, we recommend you check out the full presentation here.
Who’s qualified to answer this question?
It was a great question but not one that I am qualified to answer. But I do know someone who is at least qualified to review and comment on what information I could gather: Dr. Nathan Yost, retired pulmonary physician and building scientist (and also one of my six brothers).
Nathan worked with me at Building Science Corporation in the early 2000s, becoming one of perhaps a dozen professionals in the US to speak with authority on the relationships between indoor air quality, human health, and building science. I feel pretty lucky that I am one of a very few who can call him out of retirement on occasion for his unique expertise.
Below are the major points of discussion that Nathan and I worked up on this topic: viruses and relative humidity, with some focus on the novel coronavirus responsible for the current pandemic.
Nathan Yost’s overview
Transmission of the novel coronavirus (COVID-19) can occur in 2 ways: (1) in respiratory droplets and (2) transfer from a surface to a person’s mucous membrane (nose, eyes, or mouth), after it has been deposited on that surface from an infected person (so called face-to-hand to hand-to-face).
Transfer via respiratory droplet that are produced by normal talking and breathing requires that the two individuals come into close contact, hence the so-called “six-foot rule.” Coughing or sneezing can send viral particles beyond six feet. The good news is that the corona virus does not remain suspended in air for very long, probably a few minutes. The science of airborne pathogens is very complex. What applies to COVID-19 does not necessarily apply to other virus or even other coronaviruses.
It depends on the type of virus
Not all viruses “prefer” higher RH (that 50% – 70% shown in Figure 1). From Sterling et al: “High relative humidity tends to favor the survival of viruses composed entirely of nucleic acids and proteins, whereas lipid containing viruses prefer low relative humidities.”
The COVID 19 virus is encased in a lipid membrane so this particular virus actually prefers lower RH. And interestingly, the lipid-encased viruses are (fortunately) much more susceptible to soaps, because soaps readily break down the lipid membrane.
Manipulating RH to manage viruses
It seems there is not much research on the impact of manipulating RH to manage viruses. I could find only two studies on this topic. Here is the main takeaway from the first study:
“Preventing Airborne Disease Transmission: Review of Methods for Ventilation Design in Health Care Facilities” (November 2011; Aliabadi, Bartlett, Rogak, Green)
4.5. Viability and Infectivity
4.5.1. Pathogen Response to Environmental Conditions. The effect of environmental factors, such as temperature and relative humidity, on the survival of some aerosolized pathogens has been studied. However, the literature is limited to a few diseases, and a large class of aerosolized pathogens are yet to be analyzed. The effect of OAF [outside air filtration] (relying on natural ventilation) and electromagnetic radiation (relying on daylighting and UV disinfection) on the survival of pathogens need to be studied in greater detail. As far as the building code is concerned, the recommendations for temperature and relative humidity in functional spaces of health care facilities are very conservative. Future research should reveal more detailed mechanisms for pathogen survival behavior as a function of temperature and relative humidity so that the building code will recommend more specific environmental conditions to reduce airborne infection risk in a pathogen-specific fashion.
The second study I found also had a few takeaways:
“Humidity as a non-pharmaceutical intervention for influenza-A” (September 25 2018; Reiman, Das, Pierret)
- “Strong cyclical reduction of absolute humidity has been associated with influenza outbreaks in temperate climates.”
- “This suggests the future potential of artificial humidification as a possible strategy to control influenza outbreaks in temperate climates.”
- “One approach is to maintain relative humidity (RH) between 40–60%, the proposed optimal range for reducing growth opportunities for viruses, bacteria, and fungi. Our previous study demonstrated that classroom humidification to RH of 40–60% may be a feasible approach to increase indoor RH to levels with the potential to reduce influenza virus survival and transmission as predicted by modeling analyses.”
Nathan Yost’s perspective
Does either temperature or relative humidity affect how long the virus remains suspended in the air or viable? The answer is yes, but probably not very significant. The statement has been frequently made that the virus will “go away” once it gets warmer and more humid in April. Yes, influenza infections decrease in the spring and summer in part because that virus doesn’t live as long in humid conditions. The higher the RH the more quickly the virus falls to the floor. But human behavior also changes as weather warms—we spend more time outdoors, less time very close to other people.
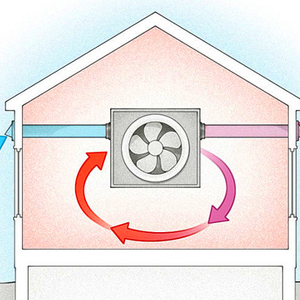
So, there probably is no reason to attempt to change the interior temperature or RH with respect to COVID-19. Maintaining RH between 35-55% minimizes the growth of many pathogens (other than COVID-19) and prevents drying of mucous membranes. Dry eyes and cracked lips affect behavior (hands touching face) and allow some viruses to more easily penetrate natural defenses. Building science is important in controlling RH throughout a building. Too much infiltration of cold, dry air can reduce RH below 35%. Poor building design or construction can create cold surfaces on which condensation occurs providing water for potential growth of fungi or bacteria.
Human-to-human vs surface-to-human transmission
Manipulating the relative humidity of indoor environments has more influence on surface-to-human transmission whereas social distancing, limiting contact, and hand washing have more influence on human-to-human transmission. The latter directly targets transmission while the former is quite indirect. And we have lots of research on the latter and very little on the former.
Nathan Yost on air purification
Why doesn’t ventilation, air filtration, or air purification make much, if any difference? The virus does not remain airborne very long and the virus does not grow on building surfaces. Unlike many bacteria and fungi, viruses grow in living cells. Yes, many viruses can remain “alive” or infectious on surfaces for hours to days, but they do not multiply on these surfaces. There is much we do not know about COVID-19 because it is a new, or novel virus. Some reports suggest that this virus can remain infectious on surfaces for up to five days. But, building materials do not provide a reservoir where the virus grows and remains for long periods of time.
Final perspective by Nathan Yost
Building science and design can play an important role in reducing infections caused by COVID-19, influenza and many viruses: reducing the number of surfaces that people touch and installing easy to clean surfaces that people will touch frequently. Think hand rails, door knobs, light switches. I love when bathroom doors at interstate rest stops have a “hook” that allows one to use ones forearm to open the door.
Keep abreast of COVID-19 updates through the Center for Disease Control.
-Peter Yost is GBA’s technical director. He is also the founder of a consulting company in Brattleboro, Vt., called Building-Wright. He routinely consults on the design and construction of both new homes and retrofit projects. He has been building, researching, teaching, writing, and consulting on high-performance homes for more than twenty years, and he’s been recognized as NAHB Educator of the Year. Do you have a building science puzzle? Contact Pete here.
Nathan Yost is a retired pulmonary physician and building scientist and Peter’s brother.
Illustration courtesy of the author.
Weekly Newsletter
Get building science and energy efficiency advice, plus special offers, in your inbox.












12 Comments
A very timely post. Thank you.
A controlled indoor environment has always been the goal of efficient housing. It will likely get more consideration now and in the future. My own house had a Honeywell electronic air cleaner when I moved here in 1993. I pulled out the cores and replaced with a 20" x 25" x 5" Merv 13 air filter. Long ago the air filter companies sized filters to replace exactly those 2 electronic cores. The original owners (built in 1978) had a good sense of indoor air quality.
Yes very interesting post.
One point of confusion:
>"Manipulating the relative humidity of indoor environments has more influence on surface-to-human transmission..."
Wasn't the discussion above that line mostly concerning RH effects on the airborne aspects of the virus? I missed the connection with how RH affects surface-to-human transfers?
On another note: There's been some social media posts circulating discussing OAF—but not 'outside air filtration' as used here, rather 'open air factor.'
I thought it was junk science at first, thinking that obviously it's just a form of ventilation which dilutes pollutants/contaminants. But it appears there may be some serious interest in it, with suggestions that its more than mere dilution (though not much conclusive evidence). A bit strange and I haven't looked into it much.
Good catch Tyler! Neither Nathan nor certainly I were familiar with this acronym/term. In the context of the reference I cited, I made the mistake of ASSUMING that OAF stood for Outside Air Filtration, when indeed Open Air Factor is a very different phenomenon.
Here is a quote from this journal article abstract
("Effect of ozone and open air factor against aerosolized Micrococcus luteus" - Journal of Food Protection, February 21, 2020)
regarding the impact of OAF:
"OAF is potentially an effective antibacterial agent that can reduce the microbial load in air. Because the technology uses reaction compounds naturally found in the environment, risks to health may be lower than those associated with ozone or other gaseous treatments. However, this hypothesis needs further investigation."
I was recently reading some information from ASHRAE distiguished lecturer, Stephanie Taylor, MD, MArch. She consults on hospital construction. Dr. Taylor recently posted on LinkedIn the following:
"Ten years ago we learned that viruses studied as surrogates for Coronavirus, the family of SARS and Wuhan, were INACTIVATED on surfaces when the ambient relative humidity (RH) was 40-60%. Conversely, when RH was either below 40% or above 60%, the viruses remained virulent and infectious.
The opportunity to inactivate viruses in the air and on surfaces by maintaining this range of indoor humidity, which happens to also be the range best for human health, is Mother Nature’s gift to us. With the excellent indoor humidification systems available, skills of building professionals, scientific acumen of microbiologists and advances in medicine, the time has come for us to co-create indoor environments truly supportive of our health."
If you read many of her posts, she places a strong emphasis on indoor humidity to reduce infection rates. Considering her qualifications and apparent experience in this area, you may wish to contact her for further insight. One of her posts "https://www.linkedin.com/pulse/ashrae-position-document-very-confusing-stephanie-h/" references over 120 studies relating to indoor conditions and infectious transmission. Dr. Taylor can be contacted through [email protected] (she shared this email in a recent post, so I don't feel badly about sharing it on the internet.)
Further, I found a couple more research papers for your reading pleasure:
https://www.condair.com/yalestudy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2863430/
https://journals.plos.org/plospathogens/article/file?id=10.1371/journal.ppat.0030151&type=printable
Thanks Yupster!
I was pretty sure that in Nathan Yost's content in this blog he made a distinction between the practicality and impact of trying to manage relative humidity in hospitals versus other buildings, with the former making sense but probably not for the latter.
I will doublecheck this with him, since it is likely that he expressed this when I interviewed him but not what I included in his write-up.
Instead of toilet paper, we're going to start seeing hygrometers flying off the shelves! ahah
Unfortunately, I live in a low performing house that is heated with a wood stove. I have developed allergies as a result. Prior to this pandemic, I have assumed that the allergies are an acceptable tradeoff until we have the financial resources to improve our home. Now, I fear that I am in the "at risk" category simply because my home has lousy indoor air quality and it has compromised my immune system and my respiratory functioning. Thus, unless I'm missing something, I think there is a substantial health benefit to having a high performing home. The occupants are, all else being equal, healthier than those of us who live in low performing homes. So when a HP home owner contracts the virus, their chance of come through unscathed is (I would think) much higher. Am I right on this? Thanks very much for your consideration.
C.X. Weiland,
Any of us can speculate, but I don't think the data exist to prove your hypothesis. The limited data that exist focus almost entirely on families that include one or more asthmatic patients. For more information, see "Housing and Human Health."
I read this interesting article and it stimulated some first principles thinking. While not being a medical professional I agree with the author that adequate humidity helps the sinuses to do their natural function of filtering microbes and viruses. The article looks at the macro environment of humidity, that is, in the home. But with the present concern over Covid-19 it seems like its wise to think about how to improve the "local" environment, the sinuses themselves. After all, with Covid-19 upon us we really can do little to affect the home RH in time to help protect ourselves.
Although the author restricted himself to building science because that is what the forum is about, maybe it's forgivable to give a more realistic solution that can be done in time to meet this crisis. That more local solution to changing the whole house is instead to purchase a nebulizer. A nebulizer is usually just a very small pump that comes with a mask and it aerosolizes either a saline solution or a medicine. The medicine is usually something similar to what is in a prescribed inhaler. A nebulizer is better than an inhaler because you can also use it with just saline (water with a salt in solution that matches the bodies own salt in solution). This can locally create exactly the conditions your sinuses need. One still has to get a prescription for the saline solution as tap water or distilled water won't work.
A nebulizer is a gold mine to have in reserve for the Corona Virus and is cheap insurance against both that and general sinus problems. The evidence that I've seen seems to show that most people wait too long to be proactive once Covid-19 symptoms appear. After two weeks from first symptom it's probably too late if symptoms haven't already resolved themselves. In other words, you'll either get better or you'll get pneumonia. Keeping your lungs clear of phlemn is a rigorous job and one that a nebulizer is made for. It also helps deliver anti-inflammatory drugs deep into the lungs when it's needed most.
Again, I'm no doctor. And you should consult your physician before taking advice. But it's better to be proactive in that first two weeks after symptoms arise. I know this is seriously off topic but I think we all know where the urgency of RH problems in homes arises from right now. There is no time for fixing that right now. Here is an interesting video from one of the earliest people to get Covid-19 in the USA. Pay careful attention to what he says at about 6:55 into the video:
https://www.youtube.com/watch?v=cFmsFHKl9g8
Edit: wrong link was put up. The new link is correct
https://www.youtube.com/watch?v=4J0d59dd-qM
Here is a corroborating video from a surgical MD explaining how complications from pneumonia is what actually kills people who have contracted Covad-19. It explains clearly the scientific mechanism that causes death. He doesn't pull his punches. Don't be offended. He's just being honest.
Do yourself a favor and watch it. The best way to help the medical profession now besides employing physical distancing from other people is to be proactive for your own health if you DO start having symptoms of Corona Virus. The best way to do that is to purchase a nebulizer "before" you need it. You can use either an isotonic or hypertonic saline solution in it to clear your lungs of phlegm. Hypertonic saline solutions are what individuals with cystic fibrosis use to clear their lungs. It can also be equally well used for the most severe symptoms of Covad-19. This will help you avoid getting pneumonia which is what ultimately kills people. You can also use doctor prescribed medicines in it that help your lungs cope with the onslaught.
I expect as people understand the usefulness of nebulizers in this pandemic that nebulizers may start to be in short supply. Don't wait. Order one. Don't expect to deserve to survive this if you have this information and you haven't acted on it. The medical system in many parts of the country will become overwhelmed quickly and early proactive actions may be your only recourse.
Great article and comments.
A good article is: Bourouiba et al., Violent expiratory events: on coughing and sneezing, Journal of Fluid Mechanics (2014), vol. 745, pp. 537-563 (MIT & PMMH - ESPCI, France).
%RH in the body/lungs can be estimated at 100%. In a low %RH environment, you essentially have a spray dryer (as we used at P&G to make powered detergents). In a low %RH environment, mass transfer occurs rapidly, within seconds, to reduce the size and mass of droplets and thereby increase droplet buoyancy. With increased buoyancy, travel distance and aloft time increase. Further, smaller droplets may penetrate deeper into the respiratory tract when inhaled, where lower respiratory tract appears to be the main target of SARS-CoV-2 infection.
From a recent article in NEJM "We found that when the person said 'stay healthy,' numerous droplets ranging from 20 to 500 μm were generated."
From Bourouiba et al.: "The ambient conditions also influence the buoyancy of the cloud and so the range of contamination of its suspended droplets. Changing the buoyancy from summer to winter indoor conditions can result in a variation of the range of deposition of the order of metres for the relatively large droplets (diameter d > 50 µm) to dozens of metres for the smallest droplets and droplet nuclei (diameter d < 10 µm). We note also that droplet evaporation can enhance the cloud buoyancy, increasing its vertical momentum and thus the chances of the cloud reaching the ceiling and contaminating the ventilation system."
And from Environment International 2020: "Airborne transmission of SARS-CoV-2: The world should face the reality". The authors ask: "Was it therefore the ventilation system that spread the airborne virus between the cabins one of the reasons for the infections?"
Isolated zones may be preferred (e.g., zoned split systems). Air purification (e.g., ozone, UV-C, vaporized hydrogen peroxide, etc.) is likely beneficial (system wide and/or local). And, as airborne transmission appears to be the main mechanism, higher humidity may help to reduce the spray dryer effect.
Various studies have identified virus RNA nearly everywhere in a hospital room (and cruise ship cabins). Finding RNA does not necessarily mean finding viable virus (size approx. 0.125 microns). It may be that people expel RNA from disrupted viruses, where such RNA is very small and can travel quite far. In crime forensics, "touch DNA" can be detected years later. Studies need to be viewed carefully as to what is actually being detected (e.g., mere RNA versus RNA as proven to be that of viable viruses).
Log in or create an account to post a comment.
Sign up Log in